Australian Asthma Handbook
The National Guidelines for Health Professionals
Recent updates
Incorrect technique when using inhaled medicines is very common among patients with asthma or COPD, with recent studies reporting as few as 10% of Australians use the correct technique. Regardless of the type of inhaler device prescribed, patients need individualised, repeated hands-on training in correct inhaler use. Our How-to video library includes demonstrations of correct technique with all the main types of inhalers, as well as spacers and nasal sprays.

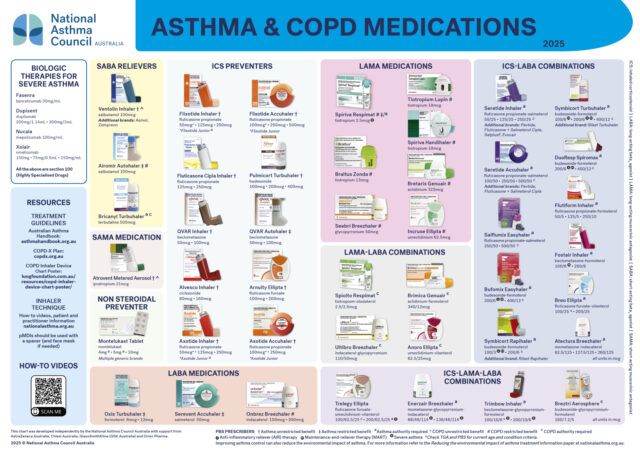
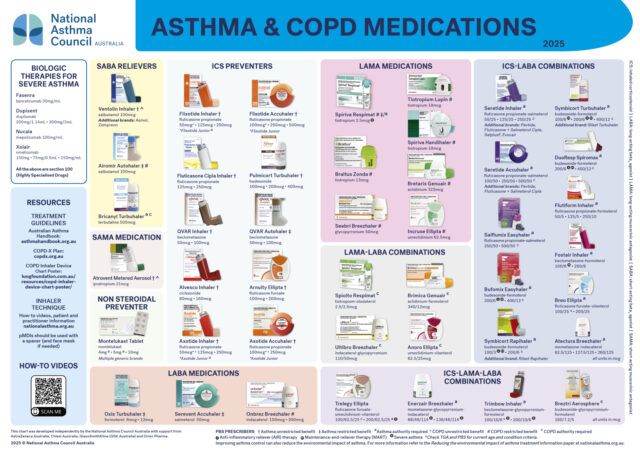
A range of evidence-based medication and spacer charts designed to go on the wall of the clinic or pharmacy to help health professionals identify and explain the range of options available. First aid charts are also available. These can be downloaded free of charge from the National Asthma Council website and are also available to order.
Questionnaire-based tools can be used to standardise review of asthma symptoms.

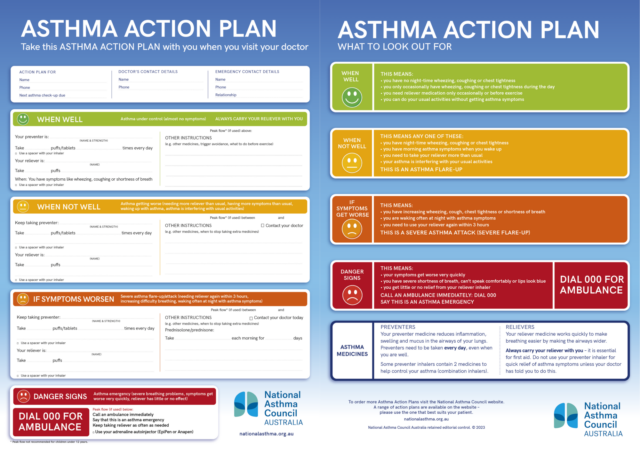
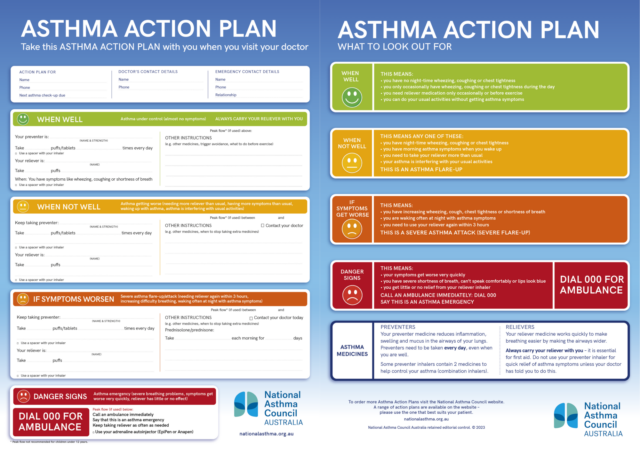
Written asthma action plans are one of the most effective asthma interventions available. An integral part of asthma management is the development of a written asthma action plan by the person with asthma and/or their carer together with their doctor.
Incorrect technique when using inhaled medicines is very common among patients with asthma or COPD, with recent studies reporting as few as 10% of Australians use the correct technique. Regardless of the type of inhaler device prescribed, patients need individualised, repeated hands-on training in correct inhaler use. Our How-to video library includes demonstrations of correct technique with all the main types of inhalers, as well as spacers and nasal sprays.

A range of evidence-based medication and spacer charts designed to go on the wall of the clinic or pharmacy to help health professionals identify and explain the range of options available. First aid charts are also available. These can be downloaded free of charge from the National Asthma Council website and are also available to order.
Questionnaire-based tools can be used to standardise review of asthma symptoms.

Written asthma action plans are one of the most effective asthma interventions available. An integral part of asthma management is the development of a written asthma action plan by the person with asthma and/or their carer together with their doctor.