Australian Asthma Handbook
The National Guidelines for Health Professionals
Tests for type 2 airway inflammation in asthma include:
FeNO and blood eosinophil count reflect different inflammatory processes and provide complementary information.[Meulmeester 2025]
Meulmeester F, Mailhot-Larouche S, Celis-Preciado C, et al. Inflammatory and clinical risk factors for asthma attacks (ORACLE2): a patient-level meta-analysis of control groups of 22 randomised trials. Lancet Respir Med 2025; 13: 505-516.
For most people with asthma, airway inflammation is driven by T helper 2 lymphocytes (type 2 inflammation).[Fahy 2015] Type 2 inflammation involves multiple inflammatory pathways leading to recruitment of eosinophils and mast cells to the airways, which results in mucus hypersecretion, airway wall oedema and thickening, and airway hyperresponsiveness.[Fahy 2015, Lambrecht 2015, Brusselle 2022] It is characterised by raised blood eosinophil counts or by raised fractional exhaled nitric oxide (FeNO) levels.[Brusselle 2022]
Two groups of patients show prominent type 2 inflammation:[Kothalawala 2020, Aaron 2018]
In other patients with asthma, airway inflammation can involve increased neutrophils, or no detected increase in granulocytes.[Brusselle 2022]
Aaron SD, Boulet LP, Reddel HK, Gershon AS. Underdiagnosis and overdiagnosis of asthma. Am J Respir Crit Care Med 2018; 198: 1012-1020.
Brusselle GG, Koppelman GH. Biologic therapies for severe asthma. N Engl J Med 2022; 386: 157-171.
Fahy JV. Type 2 inflammation in asthma–present in most, absent in many. Nat Rev Immunol 2015; 15: 57-65.
Kothalawala DM, Kadalayil L, Weiss VBN, et al. Prediction models for childhood asthma: A systematic review. Pediatr Allergy Immunol 2020; 31: 616-627.
Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol 2015; 16: 45-56.
Fractional exhaled nitric oxide (FeNO)
Inflammation of the airway, especially eosinophilic T-helper 2-driven (type 2) inflammation, is associated with increased synthesis and release of nitric oxide from airway epithelial cells.[Högman 2024]
The FeNO test is available in accredited respiratory function laboratories. The patient breathes into a mouthpiece attached to a monitor. Adults and most children aged 4–5 years and over can easily perform this test correctly.
This test is reimbursed by MBS if it is performed in an accredited respiratory function laboratory, in combination with spirometry that includes a bronchodilator responsiveness test, and is reported by a respiratory expert.
FeNO level reflects both airway inflammation and lung function changes.[Haccuria 2014]
FeNO is elevated in the presence of active type 2 inflammation of the airway associated with asthma. It is also elevated in some other inflammatory conditions (e.g. acute respiratory viral infection, allergic rhinitis/rhinosinusitis, and eosinophilic bronchitis).[GINA 2025]
FeNO is suppressed by smoking, ICS, systemic corticosteroids, and some monoclonal antibody therapies (e.g. dupilumab).[GINA 2025, Loewenthal 2022] FeNO may be normal in patients with asthma associated with types of airway inflammation (e.g. neutrophilic inflammation) and in those with obesity.[GINA 2025]
The upper limit of normal FeNO range for a population depends on age, height and sex. Development of consensus population reference ranges for the FeNO test has been limited by variation in results between measuring devices and testing protocols.[Högman 2024]
Relatively few respiratory function laboratories offer FeNO testing for children.
FeNO testing is not mandatory in the diagnostic investigation of suspected asthma in primary care and a raised FeNO level is not required to make a diagnosis of asthma. However, FeNO testing provides useful information on airway inflammation and it is increasingly used in asthma diagnosis.
When interpreted in conjunction with clinical history and results of other investigations, elevated FeNO supports a diagnosis of asthma,[Karrasch 2017] but a normal FeNO level does not rule out asthma.[Karrasch 2017]
The combination of elevated FeNO and abnormal spirometry with a positive bronchodilator responsiveness test strongly supports the diagnosis of asthma.
In adults and adolescents, FeNO ≥40 ppb supports the diagnosis of asthma in a patient with signs and symptoms strongly suggesting asthma. See Diagnosing asthma in adults and adolescents.
In children 6–11 years, FeNO ≥25 ppb supports the diagnosis of asthma in a child with signs and symptoms strongly suggesting asthma. See Diagnosing asthma in children 6-11 years.
Cut-points for the diagnosis of asthma vary between guidelines: typically 40–50 ppb for adults and 25–35 ppb for children 5–18 years. Sensitivity and specificity vary according to population.
In non-smoking patients not treated with ICS:
These sensitivities and sensitivities were calculated using a reference standard of physician diagnosis of asthma based on symptoms plus either positive bronchodilator responsiveness test on spirometry, a positive bronchial challenge test, or excessive peak flow variability.
Regular FeNO testing is not routinely required to guide asthma management in primary care.
In general, elevated FeNO helps identify patients whose asthma symptoms will respond well to ICS.[Price 2018]
The combination of blood eosinophils and FeNO might be more useful than either biomarker alone for predicting exacerbations.[Meulmeester 2025]
In patients with severe asthma, FeNO testing is commonly performed alongside blood eosinophil count to assess asthma phenotype and predict which treatment options are likely to benefit the individual. High FeNO (>25 ppb in an adult using medium-dose ICS, or >20 ppb for and adult using high-dose ICS, despite good adherence and inhaler technique[GINA 2025] in patient with poor asthma symptom control or a history of asthma exacerbation, indicates that the person may benefit from monoclonal antibody therapy. High FeNO predicts a better response to add-on treatment with dupilumab, omalizumab or tezepelumab than a lower FeNO.[GINA 2025]
BTS, NICE and SIGN. Asthma: diagnosis, monitoring and chronic asthma management (update). [F] Evidence reviews for diagnostic accuracy of fractional exhaled nitric oxide (FeNO) measures. BTS/NICE/SIGN collaborative guideline NG245. Available from https://www.nice.org.uk/guidance/ng245/evidence/f-accuracy-and-clinical-and-costeffectiveness-of-feno-in-the-diagnosis-of-asthma-pdf-13558146739
Gaillard EA, Kuehni CE, Turner S, et al. European Respiratory Society clinical practice guidelines for the diagnosis of asthma in children aged 5-16 years. Eur Respir J. 2021; 58: 2004173.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2025. Available from: www.ginasthma.org.
Haccuria A, Michils A, Michiels S, et al. Exhaled nitric oxide: a biomarker integrating both lung function and airway inflammation changes. J Allergy Clin Immunol 2014; 134: 554-9.
Högman M, Bowerman C, Chavez L, et al; Global Lung Function Initiative FENO Task Force. ERS technical standard: Global Lung Function Initiative reference values for exhaled nitric oxide fraction (FENO50 ). Eur Respir J 2024; 63: 2300370.
Karrasch S, Linde K, Rücker G, et al. Accuracy of FENO for diagnosing asthma: A systematic review. Thorax 2017; 72: 109–116.
Louis R, Satia I, Ojanguren I, et al. European Respiratory Society Guidelines for the Diagnosis of Asthma in Adults. Eur Respir J 2022; 60: 2101585.
Loewenthal L, Menzies-Gow A. FeNO in asthma. Semin Respir Crit Care Med 2022; 43: 635-645.
Meulmeester F, Mailhot-Larouche S, Celis-Preciado C, et al. Inflammatory and clinical risk factors for asthma attacks (ORACLE2): a patient-level meta-analysis of control groups of 22 randomised trials. Lancet Respir Med 2025; 13: 505-516.
Price DB, Buhl R, Chan A, et al. Fractional exhaled nitric oxide as a predictor of response to inhaled corticosteroids in patients with non-specific respiratory symptoms and insignificant bronchodilator reversibility: A randomised controlled trial. Lancet Respir Med 2018; 6: 29–39.
Global Initiative for Asthma’s overview of Type 2 biomarkers in the diagnosis and management of asthma in adolescents and adults [Appendix A]
Blood eosinophil count
Type 2 airway inflammation in patients with asthma is characterised by raised blood eosinophil levels.[Brusselle 2022]
Blood eosinophil count is also elevated in patients with atopic dermatitis [Simon 2004] and sensitised patients with recent allergen exposure.[Xu 2024]
Blood eosinophil count ≥300 cells/microlitre suggests non-asthma causes such as parasitic infestation, and very high levels (e.g. ≥1500 cells/microlitre) suggests eosinophilic granulomatosis with polyangiitis.[GINA 2025]
Levels are also influenced by sex, age, time of day, seasonality, smoking, and other conditions such as obesity and nasal polyposis, chronic infection and malignancy.[Blakey 2025]
Blood eosinophil count is not mandatory in the diagnostic investigation of suspected asthma in primary care and eosinophilia is not required to make a diagnosis of asthma.
False positive and false negative results may occur if a fixed cut-point is used for the diagnosis of asthma.[Blakey 2025]
Blood eosinophil count is not routinely required for asthma management in primary care, but is recommended in investigation of difficult-to-treat asthma (e.g. when asthma symptoms are not well controlled or the patient experiences severe exacerbations despite maintenance treatment that includes at least a medium dose of ICS).
In patients using high-dose ICS, blood eosinophil count ≥150 cells/microlitre suggests the presence of refractory type 2 inflammation.[GINA 2025]
In patients with severe asthma, blood eosinophil count is performed to assess asthma phenotype and predict which treatment options are likely to benefit the patient.[GINA 2025] It is required for PBS reimbursement for some monoclonal antibody therapies for asthma.
Higher blood eosinophil levels correlates with increased risk of asthma exacerbations.[Mallah 2021, GINA 2025] Data from several observational studies in various populations demonstrate that blood eosinophil counts ≥200 cells/microlitre are consistently associated with significantly increased risk of asthma exacerbations and severe exacerbations requiring ED visits.[Mallah 2021] The combination of blood eosinophils and FeNO might be more useful than either biomarker alone for predicting exacerbations.[Meulmeester 2025]
Blakey JD, Ramakrishnan S. Using an eosinophil count to diagnose asthma: music to your EARS? Respirology 2025; 30: 280–282.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2025. Available from: www.ginasthma.org.
Mallah N, Rodriguez-Segade S, Gonzalez-Barcala FJ, et al. Blood eosinophil count as predictor of asthma exacerbation. A meta-analysis. Pediatr Allergy Immunol 2021; 32: 465-478.
Meulmeester F, Mailhot-Larouche S, Celis-Preciado C, et al. Inflammatory and clinical risk factors for asthma attacks (ORACLE2): a patient-level meta-analysis of control groups of 22 randomised trials. Lancet Respir Med 2025; 13: 505-516.
Simon D, Braathen LR, Simon HU. Eosinophils and atopic dermatitis. Allergy 2004; 59: 561-570.
Xu X, Li J, Zhang X, et al. Blood and local eosinophil levels in chronic rhinitis: Observations during seasonal allergen exposure and non-exposure. World Allergy Organ J 2024; 17: 100930.
Global Initiative for Asthma’s overview of Type 2 biomarkers in the diagnosis and management of asthma in adolescents and adults [Appendix A]
Sputum eosinophil testing is not widely accessible in Australia. It is not used in primary care and rarely used in specialist centres.
A raised sputum eosinophil count indicates airway inflammation. In a patient using high-dose maintenance ICS treatment, sputum eosinophil count ≥2% suggests the presence of refractory type 2 inflammation.[GINA 2025]
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2025. Available from: www.ginasthma.org.
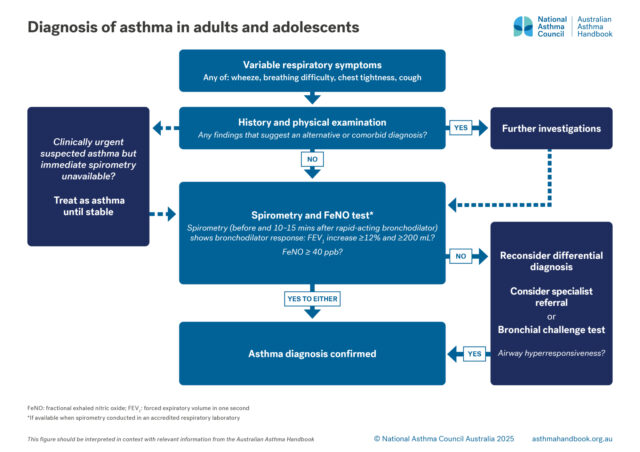
Adults and Adolescents
Investigation of suspected asthma and diagnostic criteria in adolescents and adolescents.
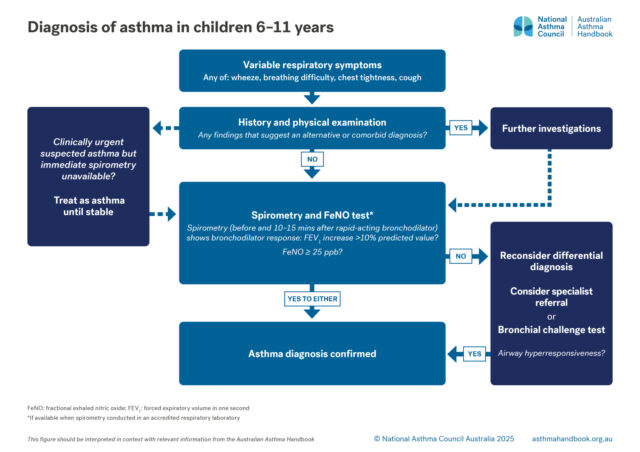
Children 6-11 years
Investigation of suspected asthma and diagnostic criteria in children 6–11.
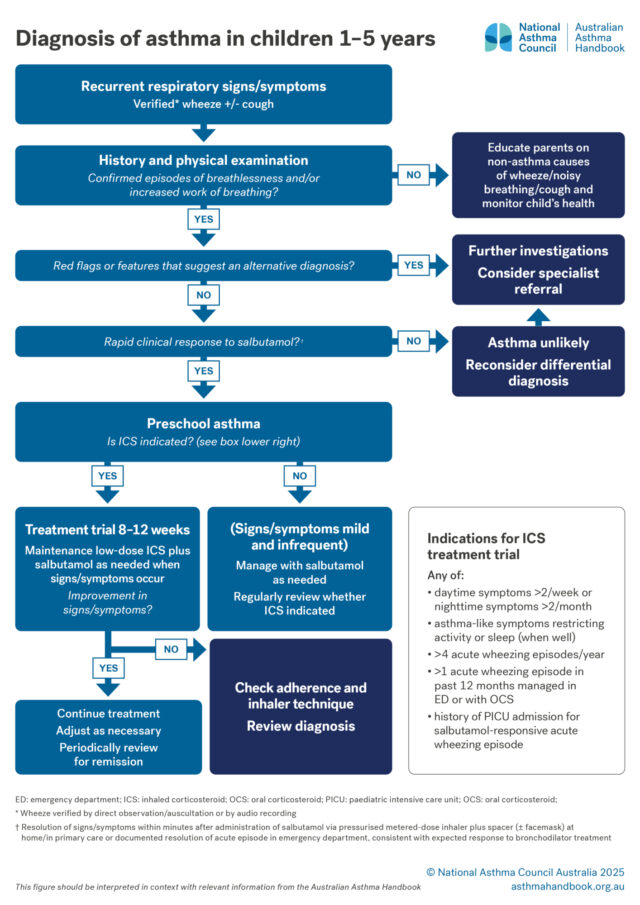
Children 1-5 years
Investigation of suspected asthma and diagnostic criteria in preschool children.